Điều trị tăng sắc tố sau viêm bằng laser là vấn đề lớn được đặt ra hiện nay vì đôi khi làm nặng thêm tình trạng PIH. Hy vọng qua bài tổng kết này các đồng nghiệp đang làm việc ở các Trung tâm Thẩm mỹ sẽ có cái nhìn tổng quát hơn để áp dụng trong điều trị laser
Clinical Review& Education
JAMADermatology | Review
Laser Treatments for Postinflammatory Hyperpigmentation A Systematic Review
Oma Agbai, MD; Iltefat Hamzavi, MD; Jared Jagdeo, MD
Author Affiliations: Department of Dermatology, University of California, Davis, Sacramento (Agbai, Jagdeo); Department of Dermatology, Henry Ford Hospital, Detroit, Michigan (Hamzavi); Dermatology Service, Sacramento Veterans Affairs Medical Center, Mather, California (Jagdeo); Department of Dermatology, State University of New York Downstate Medical Center, Brooklyn (Jagdeo). Corresponding Author: Oma Agbai, MD, Department of Dermatology, University of California, Davis, 3301 C St, Ste 1400, Sacramento, CA 95816

IMPORTANCE Lasers are gaining interest as a treatment option for postinflammatory hyperpigmentation (PIH) but can pose a clinical dilemma given the risk for laser-induced or exacerbated PIH.
OBJECTIVE To assess the clinical evidence for the use of lasers in the treatment of PIH.
EVIDENCE REVIEW A systematic review was performed by searching PubMed databases from January 1, 1990, through May 31, 2016. Included studies involved laser treatment for PIH with the degree of pigmentation as a measure of outcome. The search was filtered to include only clinical studies written in the English language. Study methods were analyzed and the reproducibility of the studies was graded. Outcome measures varied from study to study and included concentration of melanin and hemoglobin, patient satisfaction questionnaires, clinical photography, subjective clinical improvement, light microscopy, melanin index, reflectance spectroscopy, and/or skin biopsy evaluated by a blinded dermatopathologist.
FINDINGS Of 1295 results, 20 unique studies with 224 patients met the inclusion criteria. These studies included 1 randomized clinical observer-blinded study (6 patients), 4 nonrandomized clinical trials (133 patients), 1 cohort study (34 patients), 7 case series (44 patients), and 7 case reports (7 patients). Multiple lasers were studied; however, most of the studies were not methodologically rigorous. Some studies showed no improvement or worsening of PIH after laser treatment. The most extensively studied device was the Q-switched Nd:YAG laser, which has shown promising results based on multiple outcome measures as listed above.
CONCLUSIONS AND RELEVANCE Some lasers may be beneficial in the treatment of PIH. The evidence suggests that additional studies would be required to determine the benefit of laser treatment of PIH.
JAMA Dermatol. doi:10.1001/jamadermatol.
Key Points
Question Do effective laser treatments for postinflammatory hyperpigmentation exist?
Findings In this systematic review, multiple lasers were studied; however, most of the studies were not methodologically rigorous, and some studies showed no improvement or worsening of postinflammatory hyperpigmentation after laser treatment. The most extensively studied device in our review, the Q-switched Nd:YAG laser, has shown promising results.
Meaning Some lasers may be beneficial in the treatment of postinflammatory hyperpigmentation, but evidence suggests that additional studies would be required to determine the benefit of laser treatment of postinflammatory hyperpigmentation.
Postinflammatory hyperpigmentation (PIH) is a reactive cutaneous hypermelanosis caused by an inflammatory process, such as eczema, acne, trauma, or cosmetic procedures. Postinflammatory hyperpigmentation is a very common complaint, especially among people of color, often causing significant psychological stress and severely affecting the patient’s quality of life. A vast array of treatment options is available for managing PIH, ranging from topical applications to chemical peels to laser treatments. Although topical treatments remain the standard of care for treating PIH, lasers are gaining interest as a treatment option and are being evaluated in a small number of clinical studies with limited rigor. Herein, we will discuss the studies evaluating the efficacy of the multiple lasers in PIH treatment that meet our inclusion and exclusion criteria.
METHODS
We searched PubMed databases for published clinical studies examining the use of lasers for treating hyperpigmentation from January 1, 1990, through May 31, 2016. Search terms included laser post-inflammatory hyperpigmentation, laser postinflammatory hyperpigmentation, and laser hyperpigmentation. We included studies that involved laser treatment for PIH with the degree of pigmentation as a measure of outcome. We filtered our search to include only clinical studies published in English. Searches were also filtered to exclude PIH of themucosal surfaces. Additional exclusion criteria consisted of cases of hyperpigmentation believed to be secondary to hemosiderin deposition. We included studies on PIH in the setting of suspected increased melanin deposition. We searched bibliographies for additional studies that met inclusion and exclusion criteria. Of 1295 results, 20 unique studies with 224 patients met the inclusion criteria. Quality of evidence was graded on a scale of 1 to 5, where 1 indicates a properly powered and conducted randomized clinical trial or a systematic review with meta-analysis; 2, a well-designed controlled trial without randomization or a prospective comparative cohort trial, 3, a case-control study or a retrospective cohort study; 4, a case series with or without intervention or a cross-sectional study; and 5, an opinion of respected authorities or case reports.1 The PRISMA diagram is given in the Supplement.
RESULTS
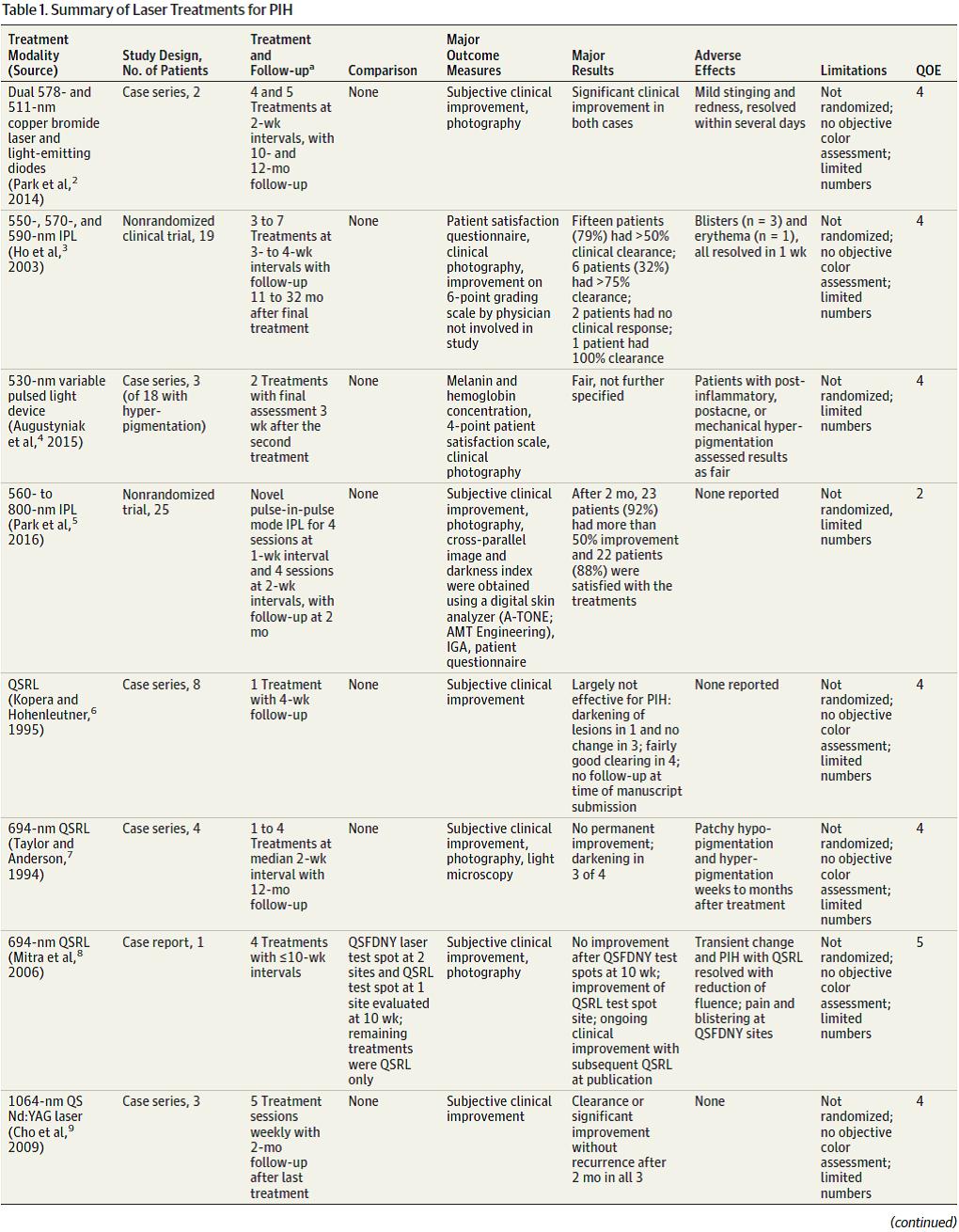
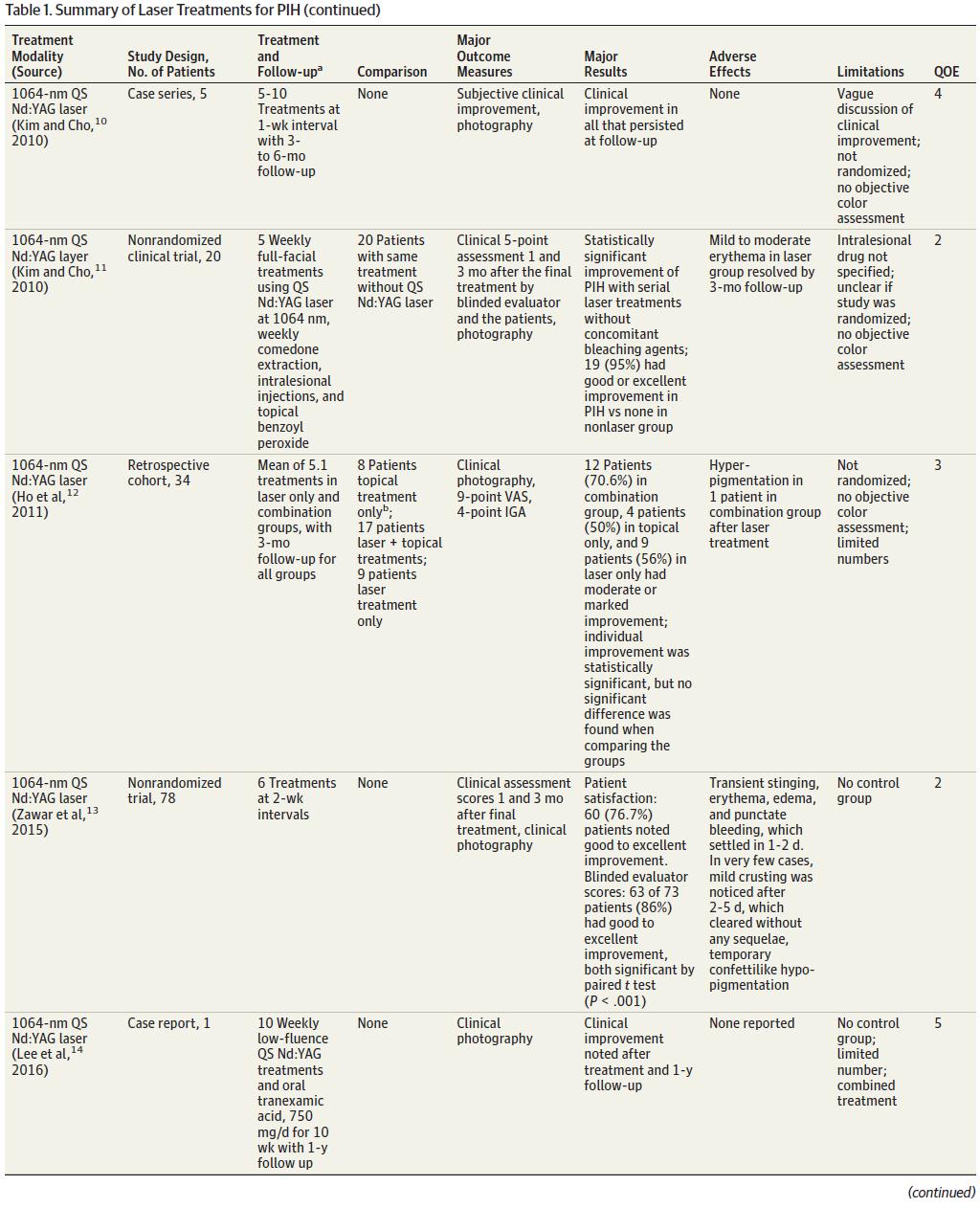
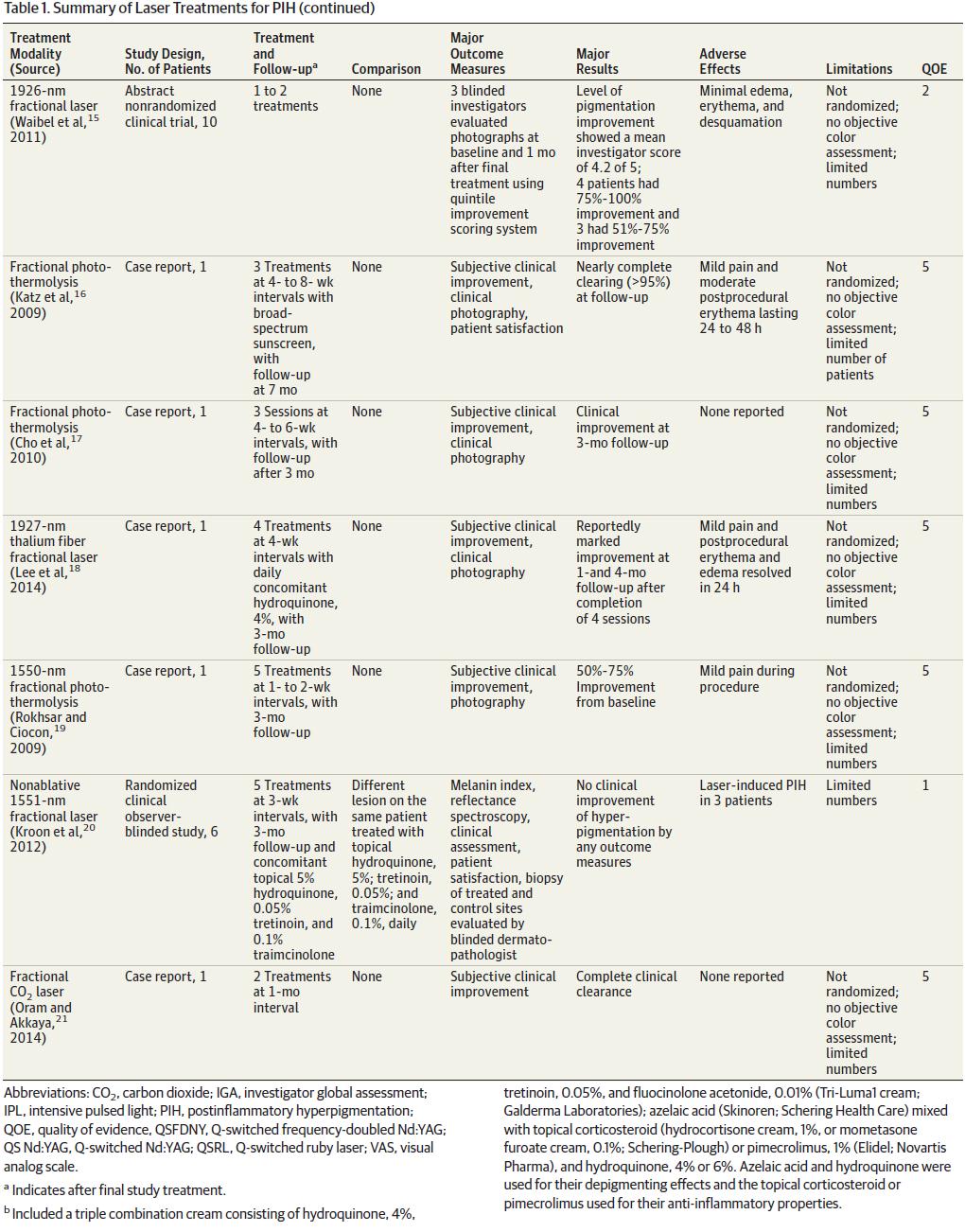
Of 1295 results, 20 studies met the inclusion criteria and are summarized in Table 1. These included 1 randomized clinical observerblinded study,20 4 nonrandomized clinical trials,5,11,13,15 1 cohort study, 7 case series,2-4,6,7,9,10 and 7 case reports.8,14,16-19,21 Six patients participated in the randomized clinical observer-blinded study; 133, in nonrandomized clinical trials; 34, in cohort studies; 44, in case series; and 7, in case reports, for a total of 224 patients. Types of laser treatments for PIH included the dual 578- and 511-nm copper bromide laser and light-emitting diodes2; 550-, 570-, and 590-nm intense pulsed light3; 694-nm Q-switched ruby laser (QSRL)6-8; 1064-nm QS Nd:YAG9-12; fractional photothermolysis15-20; and fractional carbon dioxide modalities.21
Copper Bromide Laser and Light–Emitting Diodes
Park and colleagues2 reported 2 cases of PIH treated by combined 578- and511-nmcopperbromide laser andlight-emittingdiodes.The patients underwent 4 and 5 sessions at 2-week intervals, and the authors reported significant clinical improvement in both cases. Adverse effects included mild stinging and redness.
Intense Pulsed Light
Hoandcolleagues3 performedanonrandomizedclinical trial toevaluate the efficacy of 550-, 570-, and 590-nm intense pulsed light as a treatment option for PIH. Nineteen patients underwent 3 to 7 treatments at intervals of 3 to 4 weeks. Outcome measures included a patient satisfaction questionnaire, clinical photography, and improvement assessed with a 6-point grading scale by a blinded physician. Fifteen patients (79%)showedmorethan50%clearance. Six patients (32%)had more than 75%clearance. Two patients showed no clinical response, and 1 patient had100%clearance. Adverse effects were transient and included blisters in 3 patients and erythema in 1. All adverse effects resolved within 1 week. In a study performed by Augustyniak and colleagues,4 a variable pulsed light device was used to treat 18 patients with various disorders of hyperpigmentation, including 3 patients with PIH. The remaining participants had hyperpigmentation resulting from various causes ranging from melasma to thyroid disease. A reflectance tool (Mexameter MX 18; CK Electronic GmbH) was used to measure the concentration of melanin and hemoglobin. Furthermore, patient satisfactionwas assessed at 3-week intervals using a 4-point scale. The researchers demonstrated a statistically significant improvementin 13 of the 18 patients. With regard to the 3 patients with PIH, resultswere reported as fair without further specification. Adverse effects included worsening of pigmentation.4
Q-Switched Ruby Laser
Three studies evaluated the efficacy of the QSRL in the treatment of PIH. Kopera and Hohenleutner6 reported a series of 8 cases in which each patient underwent one 694-nm QSRL treatment with a 4-week follow-up. Subjective clinical improvement was the primary outcome measure. The authors concluded that the QSRLwas not effective in treating PIH.
Similarly, Taylor and Anderson7 reported 4 cases of PIH treated with a 694-nm QSRL. Patients underwent 1 to 4 treatments
at a median interval of 2 weeks and clinical follow-up after 12 months. Outcome measures included subjective clinical improvement, clinical photography, and histologic examination by light microscopy. At the 12-month follow-up, no significant
improvement was noted in any patients, and darkening was seen in 3 of 4 subjects. Adverse effects included patchy hypopigmentation and hyperpigmentation at sites of treatment. This finding persisted weeks to months after treatment.
Mitra and colleagues8 reported 1 case of QSRL treatment for PIH. Four treatments were performed at intervals as long as 10
weeks. Outcome measures included subjective clinical improvement and clinical photography. At the beginning of the study, test spots were performed on 1 site using a QSRL and on 2 sites using a Q-switched, frequency-doubled, Nd:YAG (QSFDNY) laser. At the 10-week follow-up, the investigators noted no subjective clinical improvement on the QSFDNY-treated sites but noticed lightening of PIH on the QSRL-treated site. The authors thus proceeded with 4 QSRL treatments of varying intervals, lasting as long as 10 weeks. The authors reported progressive clinical improvement of the sites undergoing QSRL treatment by the time of publication. The only adverse effects reported included transient PIH. Pain
and blistering occurred at the test spots treated with the QSFDNY laser.8
Q-Switched Nd:YAG Laser
The QS Nd:YAG laser has also been studied by multiple investigators. A case series by Cho and colleagues9 reported on a series of 3 cases of PIH undergoing 1064-nmQSNd:YAGtreatment. These patientswere treated with5weekly sessions,and clinical follow-up was performed 2 months after the final treatment. Main outcome measures included subjective clinical improvement. The authors reported clearance or significant improvement in all 3 patients without recurrence at follow-up. No major adverse effects were reported.9 Similarly, Kim and Cho10 reported a series of cases of PIH undergoing 1064-nm QSNd:YAGtreatment. Five patients in the study underwent 5 to 10 treatments at 1-week intervals, and clinical follow-up was performed 3 to6months after the final treatment. Out-come measures included subjective clinical improvement and clinical digital photography.Theauthors reported that all treated patients experiencednoticeableclinical improvement thatpersistedat followup. No adverse effects were reported. The same year,KimandCho11 published a nonrandomized clinical trial of 20 patients in a treatment group receiving 5weekly full-facial 1064-nm QS Nd:YAG treatments for acne-induced facial PIH.
For acne, the laser treatment group also underwent weekly comedone extraction, intralesional injections (injected drug was not specified), and topical benzoyl peroxide application. The comparison group consisted of 20 patients who also underwent 5 weekly treatments ofcomedoneextraction, intralesional injections,andtopi-cal benzoyl peroxide application. This comparison group did not undergo laser treatment. Outcome measures included a 5-point clinical assessment of digital photographs by a blinded evaluator 1 and 3 months after the final treatment and clinical photography. The investigators reported that serial laser treatments without concomitant use of bleaching agents resulted in statistically significant improvement of PIH. Improvementof PIHwas graded on the following scale: none (0 improvement; 1 point), poor (1%-24% improve-ment;2points), fair (25%-49%improvement;3points),good(50%-74%improvement; 4 points), and excellent (75%-100% improvement;5 points). Twenty patients (95%) had good or excellent improvement in PIH as rated by a blinded observer compared with none achieving this rating in the nonlaser group. Adverse effects included mild to moderate erythema in the laser group, which all resolved by follow-up at 3 months. Ho and colleagues12 performed a historically controlled study evaluating 34 patients who were treated for PIH using various modalities and divided them into groups that received (1) topical treatments only, (2) laser and topical treatments, and (3) laser treatments only. Topical treatments included a triple combination creamconsisting of hydroquinone, 4%, tretinoin, 0.05%, and fluocinolone acetonide, 0.01%(Tri-Luma 1 cream; Galderma Laboratories); azelaic acid (Skinoren; Schering Health Care) mixed with topical corticosteroid (hydrocortisone cream, 1%, or mometasone furoate cream, 0.1%; Schering-Plough); or pimecrolimus, 1% (Elidel; Novartis Pharma), and hydroquinone, 4% or 6%. Azelaic acid and hydroquinone were used for their depigmenting effects, and the topical corticosteroid and pimecrolimus were used for their anti-inflammatory properties. The lasers used for managing PIH were the 595-nm long pulsed-dye laser (VBeam; Candela Corporation) and/or the 1064-nm QS Nd:YAG laser (MedLite C3 or C6; Hoya ConBio Inc). The long pulsed-dye laser was used primarily to target the vascular component of the acne dyspigmentation, and the QS Nd:YAG laser was used to target the pigmentary component. Outcome measures included clinical photography, a 9-point visual analog scale, and a 4-point investigator global assessment of improvement. The investigator global assessment was performed by a blinded independent clinician and consisted of a grading system based on clinical pretreatment and posttreatment photographs where 0 indicates worsening; 1, no change; 2, mild improvement; 3, moderate improvement; and 4, marked improvement. Twelve patients (71%) in the combination treatment group had moderate or marked improvement, compared with 4 patients (50%) in the topical treatment group. The authors reported that improvement within each group was statistically significant, but that no statistical significance was found when comparing the groups with one another. Reported adverse effects included hyperpigmentation in 1 patient in the combination treatment group after a laser treatment.
Fractional Laser
Waibel and colleagues15 performeda nonrandomized clinical trial involving 10 patients who underwent 1 to 2 treatments of a 1926-nm laser for treatment of PIH.Three blinded investigatorsevaluated clinical photographs at baseline and 1 month after the final treatment.
Scores were assigned using a quintile improvement scoring system. The investigator score for level of improvement was 4.2 of 5. Four patients (40%) had 75% to 100% improvement. Three patients (30%) had 51% to 75% improvement. Adverse effects included minimal erythema, edema, and desquamation.
Katz and colleagues16 reported a case of 1 patient who underwent 3 treatments of fractional photothermolysis at 4- to 8-week intervals. Broad-spectrum sunscreenwas applied during the course of treatment. Outcome measures included subjective clinical improvement and clinical photography. Patient satisfaction was also assessed through aquestionnaire.The investigators reported nearly complete clearing (>95%) at the 7-month follow-up. Adverse effects included mild pain and moderate postprocedural erythema lasting 24 to 48 hours.16
Cho and colleagues17 reported a case of 1 patient treated with a fractional photothermolysissystemat4- to6-week intervalsusing a pulsed light and laser system (StarLux 1540TM; Palomar Medical Technologies, Inc). Follow-up evaluation was performed 3 months after the final treatment. Outcome measures included subjective clinical improvement and clinical photography. The authors reported subjective clinical improvement at the 3-month follow-up appointment. No adverse effects were reported.17
Lee and colleagues18 reported 1 case of cupping-induced PIH treated with a 1927-nm fractional laser after application of hydroquinone cream,4%,for4months failed to showimprovement. Four treatments were performed at 4-week intervals, and daily hydroquinone cream, 4%,was applied during the treatment period. Outcome measures included subjective clinical improvement and clinical photography. The investigators reported marked improvement at 1 and4months after the final treatment had been completed. Adverse effects included mild pain and postprocedural erythema and edema, which all resolved within 24 hours.18
Rokhsar and Ciocon19 reported a case of 1 woman who was treated with 1550-nm fractional photothermolysis to treat PIH caused by a carbon dioxide laser. Five treatments were performed at 1-week intervals with a 3-month follow-up. Outcome measures included subjective clinical improvement and clinical photography.
The authors reported 50% to 75% improvement from baseline. Adverse effects included mild pain during the procedure.19
Kroon and colleagues20 performed a randomized clinical observer-blinded study evaluating the efficacy of a 1551-nm nonablative fractional laser in 6 patients with PIH. For each patient, 2 similarly affected areas were randomized to undergo 5 nonablative fractional laser treatments at 3-week intervals combined with topical hydroquinone, 5%, tretinoin, 0.05%, and triamcinolone acetonide, 0.1%, or daily topical therapy only consisting of topical hydroquinone, 5%, tretinoin, 0.05%, and triamcinolone, 0.1%. Outcome measures included the melanin index, reflectance spectroscopy, clinical assessment, patient satisfaction, and biopsy of treated and control sites evaluated by a blinded dermatopathologist. From these studies the authors found no statistically significant clinical improvement in the study group treated with combined laser and topical therapy. Adverse effects included laserinduced PIH in 3 patients.20
Oram and Akkaya21 reported a case of 1 patient treated with a fractional carbon dioxide laser. Two treatmentswere performed at a 1-month interval. Subjective clinical improvement was the primary outcome measure. The authors reported complete clinical clearance at the follow-up appointment.
DISCUSSION
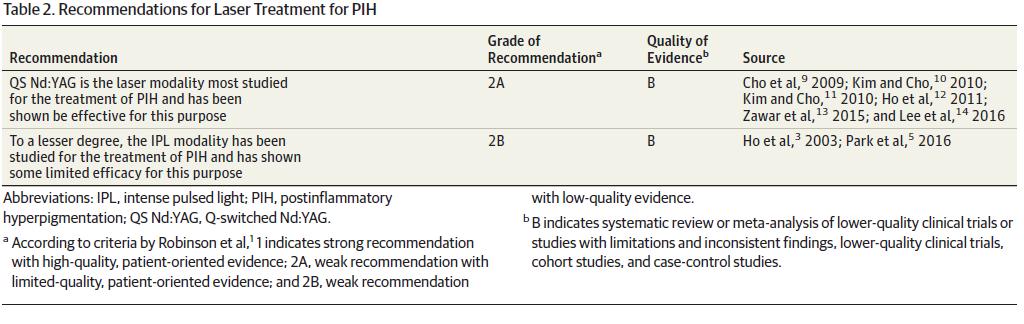
Postinflammatory hyperpigmentation is an acquired hypermelanosis of the skin that may be triggered by any antecedent inflammation or injury. Its incidence ismorecommonin darker skin types. With the emergence of laser treatments in dermatology in recent years and the wide absorption spectrum of melanin as a chromophore, a variety of lasers has been studied as potential treatment of PIH. In Table 1, the 20 included studies evaluating laser treatment of PIH are graded on a scale from 1 to 5 based on quality of evidence, where 1 indicates the best evidence.1 Table 2 provides recommendations based on these ratings. One randomized clinical observer-blinded study20 evaluating the use of a nonablative 1551-nm fractional laser reached level 1. This study was also unique in that objective outcome measures, such as melanin index reflectance spectroscopy and histologic analysis by a blinded dermatopathologist, were used. Of note, no statistically significant improvement was seen in any of the outcome measures, which also included clinical assessment and a patient satisfaction questionnaire. Furthermore, laser-induced PIH was observed in 3 of 6 patients. Although several clinical studies are highlighted herein, additional therapies for PIH involving laser management may be available that have yet to be studied. For example, the authors have observed that the long-pulsed Nd:YAG laser may be efficacious in treating PIH, because patients undergoing laser hair reduction with a long-pulsed Nd:YAG laser have shown lightening of PIH associated with pseudofolliculitis barbae (Figure). Potential reasons for this observation include gradual lightening of PIH in the setting of improved pseudofolliculitis barbae, which may occur independently of the laser treatments. However, we do not have enough information to exclude a potential therapeutic effect of the long-pulsed Nd:YAG laser therapy on PIH. This area has not been formally studied, to our knowledge, and warrants further in-depth investigation.
CONCLUSIONS
The use of lasers for treating PIH is a controversial topic lacking large randomized clinical trials. A number of other factors pose limitations in the reviewed clinical studies. For example, concomitant use of other depigmenting agents is not controlled for in most cases. In addition, to our knowledge, none of the studies controlled for the intensity of normal pigmentation, which can affect the degree of PIH and perhaps the relative improvement with treatment. None of the studies used a validated scoring system for acne-induced PIH as suggested by Savory et al.22 Furthermore, the diagnosis of PIH was not confirmed histologically in most cases. In addition, the studied patients represent a wide variety of Fitzpatrick skin types. Therefore, the treatment response of a lighter skin type does not predict the response of a darker skin type, in which the incidence of PIH is most prevalent and often more severe. Several studies lacked control comparison groups. Finally, studies reviewed herein generally involve cases of PIH refractory to other treatments, which may result in a selection bias for severe cases that may not be representative of most PIH cases. Further studies including larger patient populations are indicated to fully characterize the clinical utility of laser treatments for PIH.
REFERENCES
1. Robinson JK, Dellavalle RP, Bigby M, Callen JP. Systematic reviews: grading recommendations and evidence quality. Arch Dermatol. 2008;144(1):97-99.
2. Park KY, Choi SY, Mun SK, Kim BJ, Kim MN. Combined treatment with 578-/511-nm copper bromide laser and light-emitting diodes for
post-laser pigmentation: a report of two cases.
Dermatol Ther. 2014;27(2):121-125.
3. HoWS, Chan HH, Ying SY, Chan PC, Burd A, King WW. Prospective study on the treatment of postburn hyperpigmentation by intense pulsed
light. Lasers Surg Med. 2003;32(1):42-45.
4. Augustyniak A, Erkiert-Polguj A, Rotsztejn H. Variable pulsed light treatment of melasma and post-inflammatory hyperpigmentation: a pilot
study. J Cosmet Laser Ther. 2015;17(1):15-19.
5. Park JH, Kim JI, KimWS. Treatment of persistent facial postinflammatory hyperpigmentation with novel pulse-in-pulse mode intense pulsed light.
Dermatol Surg. 2016;42(2):218-224.
6. Kopera D, Hohenleutner U. Ruby laser treatment of melasma and postinflammatory hyperpigmentation. Dermatol Surg. 1995;21(11):994.
7. Taylor CR, Anderson RR. Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser.
J Dermatol Surg Oncol. 1994;20(9):592-597.
8. Mitra A, Yeung R, Sheehan-Dare R, Wilson CL. Lentiginous hyperpigmentation confined to resolved psoriatic plaques and treated with a Q-switched ruby laser. Clin Exp Dermatol. 2006;31 (2):298-299.
9. Cho SB, Park SJ, Kim JS, Kim MJ, Bu TS. Treatment of post-inflammatory hyperpigmentation using 1064-nm Q-switched Nd:YAG laser with low fluence: report of three cases. J Eur Acad Dermatol Venereol. 2009;23(10): 1206-1207.
10. Kim S, Cho KH. Treatment of procedure-related postinflammatory hyperpigmentation using 1064-nm Q-switched Nd:YAG laser with low fluence
in Asian patients: report of five cases. J Cosmet Dermatol. 2010;9(4):302-306.
11. Kim S, Cho KH. Treatment of facial postinflammatory hyperpigmentation with facial acne in Asian patients using a Q-switched neodymium-doped yttrium aluminum garnet laser. Dermatol Surg. 2010;36(9):1374-1380.
12. Ho SG, Yeung CK, Chan NP, Shek SY, Kono T, Chan HH. A retrospective analysis of the management of acne post-inflammatory hyperpigmentation using topical treatment, laser treatment, or combination topical and laser treatments in oriental patients. Lasers Surg Med.
2011;43(1):1-7.
13. Zawar VP, Agarwal M, Vasudevan B. Treatment of Postinflammatory pigmentation due to acne with Q-switched neodymium-doped yttrium aluminum garnet in 78 Indian cases. J Cutan Aesthet Surg. 2015;8(4):222-226.
14. Lee YB, Park SM, Kim JW, Yu DS. Combination treatment of low-fluence Q-switched Nd:YAG laser and oral tranexamic acid for post-inflammatory hyperpigmentation due to allergic contact dermatitis to henna hair dye. J Cosmet Laser Ther. 2016;18(2):95-97.
15. Waibel J,Wasserman D, Houshmand E, Tierney E. Treatment of post-inflammatory hyperpigmentation with 1927 nm thulium fractional laser [published online February 15, 2011]. Lasers Surg Med. doi:10.1002/lsm.21034
16. Katz TM, Goldberg LH, Firoz BF, Friedman PM. Fractional photothermolysis for the treatment of postinflammatory hyperpigmentation. Dermatol Surg. 2009;35(11):1844-1848.
17. Cho SB, Lee SJ, Kang JM, Kim YK, Oh SH. Treatment of refractory arcuate hyperpigmentation using a fractional photothermolysis system.
J Dermatolog Treat. 2010;21(2):107-108.
18. Lee SJ, ChungWS, Lee JD, Kim HS. A patient with cupping-related post-inflammatory hyperpigmentation successfully treated with a 1,927 nm thulium fiber fractional laser. J Cosmet Laser Ther. 2014;16(2):66-68.
19. Rokhsar CK, Ciocon DH. Fractional photothermolysis for the treatment of postinflammatory hyperpigmentation after carbon dioxide laser resurfacing. Dermatol Surg. 2009;35 (3):535-537.
20. KroonMW, Wind BS, Meesters AA, et al. Non-ablative 1550 nm fractional laser therapy not effective for erythema dyschromicum perstans and
postinflammatory hyperpigmentation: a pilot study. J Dermatolog Treat. 2012;23(5):339-344.
21. Oram Y, Akkaya AD. Refractory postinflammatory hyperpigmentation treated fractional CO2 laser. J Clin Aesthet Dermatol. 2014;7
(3):42-44.
22. Savory SA, Agim NG, Mao R, et al. Reliability assessment and validation of the Postacne Hyperpigmentation Index (PAHPI), a new instrument to measure postinflammatory hyperpigmentation from acne vulgaris. J Am Acad Dermatol. 2014;70(1):108-114.
Downloaded From: http://jamanetwork.com/ by a World Health Organization User on 01/05/2017