'COVID Toes' and 'Kawasaki' Rash: 5 Cutaneous Signs in COVID-19
Graeme M. Lipper, MD
DISCLOSURES
May 08, 2020
Find the latest COVID-19 news and guidance in Medscape's Coronavirus Resource Center.
The skin manifestations of the novel coronavirus SARS-CoV-2 were not recognized at the early stages of the pandemic but have received much recent attention in scientific journals and global media outlets. Reported manifestations range from pseudo-chilblains to a morbilliform (measles-like) exanthem, urticaria, vesicular eruptions, a dengue-like petechial rash and ovate scaling macules, and plaques mimicking pityriasis rosea.
The New 'Great Mimicker'
Much like with HIV and syphilis, COVID-associated "rashes" seem to be as numerous as they are hard to pin down. The largest published study to date is a nationwide case series in Spain with 375 cases which identified five clinical patterns. Because of the scarcity and low sensitivity of diagnostic tests available, the investigators accepted patients with confirmed disease as well as those with a clinical diagnosis of COVID in the study. Just under half (41%) of patients with pseudo-chilblains had confirmed infection with positive viral cultures and/or serology.
Observed COVID-associated skin patterns were:
These investigators found that the vesicular eruptions appeared earliest in the course of COVID-19, prior to any other symptoms in 15% of cases; these developed on the trunk and extremities, were most common in middle-aged adults, and typically lasted around 10 days.
In contrast, the pseudo-chilblains eruption which has received much attention on social media (using the hashtag #COVIDtoes) occurred later. In almost two thirds (59%) of patients, these lesions developed after other symptoms. Despite much concern in the lay press about lesions on toes (which can also, less frequently, present on fingers), pseudo-chilblains acral lesions correlated with a milder disease course and younger patient age. Livedo and necrosis, however, indicated more severe illness and a poor prognosis.
Patients with maculopapular exanthems (47% of reported cases in this series) also had more severe infections and typically manifested skin findings at the same time as other COVID-19 symptoms.
Sounding the Alarm in Kids
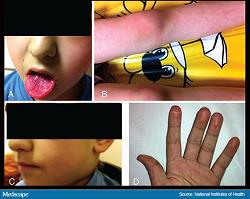
In a recent and alarming twist, more than a dozen children—the group once thought to be most immune to severe COVID complications—have presented in the United Kingdom with a multisystem inflammatory condition with features of toxic shock syndrome and atypical Kawasaki disease. Kawasaki-like signs of this "SARS-CoV-2-related inflammatory syndrome" include an erythematous rash, conjunctivitis and glossitis with high fever, abdominal pain and gastrointestinal symptoms, and cardiac inflammation. Another 25 children with similar findings have been identified in France.
Some of these children have tested SARS-CoV-2 positive or had serologic evidence of prior SARS-CoV-2 infection. These findings prompted a warning from the National Health Service and the Paediatric Intensive Care Society.
A similar alert was just issued by the New York City Health Department after 15 children, ages 2-15, were hospitalized in NYC between April 17 and May 1 with illnesses compatible with this syndrome (ie, typical Kawasaki disease, incomplete Kawasaki disease, and/or shock). Polymerase chain reaction (PCR) testing for SARS-CoV-2 was positive in four of the NY children. As of May 6, 2020, the reported number of children affected in New York had risen to 64 and cases in other states were reported.
COVID Toes



Of all the COVID-associated skin manifestations, pseudo-chilblains has drawn the most attention to date. "COVID toes" were first described in China and then in Europe by a network of dermatologists in Italy, Spain, Belgium, and France. These cases typically affect children and young adults, manifesting as acro-located erythematous to violaceous papules and plaques primarily affecting the toes and mimicking chilblains (idiopathic pernio).
Classic cold-induced chilblains is a benign and self-limited condition characterized by acral erythema of the toes (and sometimes fingers) with swelling. In contrast, pseudo-chilblains (COVID toes) often occurs in warmer climates, tends to be more severe and symptomatic (itching, burning, pain), is more likely to ulcerate, and takes longer to resolve.
The earliest case series describing "acro-ischemia presentations" included finger and toe cyanosis, skin bullae, and dry gangrene. This Chinese case series looked at seven critically ill patients with COVID-19 pneumonia, diagnosed and treated in Wuhan in early February. In addition to having fever, cough, and dyspnea, all of the patients developed finger and/or toe cyanosis which progressed to bullae, skin ulceration, and necrosis. All of these individuals also had evidence of a hypercoagulable state with elevated D-dimers and fibrinogen degradation products, and prolonged prothrombin times. Despite treatment with low-molecular-weight heparin, these patients had a poor prognosis; five died with a median time from acro-ischemia onset to death of 12 days.
In contrast, the reported cases of pseudo-chilblains coming out of Europe, the Middle East, and the United States fit more into the benign pattern described by researchers in Spain.
A recent paper described a case involving a 23-year-old man. He presented with sudden-onset "violaceous, infiltrated, and painful plaques on the toes and lateral aspect of the feet," preceded by fever and a dry cough. This patient had no prior history of chilblains, Raynaud's phenomenon, or collagen vascular disease. A nasopharyngeal swab tested PCR-positive for SARS-CoV-2, and coagulation studies were normal with no D-dimers. Histopathology was similar to that of idiopathic pernio, showing a small-vessel lymphocytic vasculitis with variable levels of papillary dermal edema and no intravascular thrombi.
Anecdotally, most young patients with pseudo-chilblains seem to follow this benign course, often remaining otherwise asymptomatic. Adding to the uncertainty, some with clinical features and a history highly suggestive of COVID-related pseudo-chilblains have tested SARS-CoV-2-negative by PCR and/or serologies.
Discussion
The story of COVID-19 and skin manifestations is changing every day, with dozens of papers still in press. While the spotlight has fallen on pseudo-chilblains ("COVID toes"), the pathophysiology behind this strange manifestation remains mysterious. Some question whether this is a true COVID manifestation or merely an epiphenomenon—so-called "quarantine toes"—brought about by more people walking barefoot during quarantine and an unusually cold spring in parts of the United States.
Some cases may indeed be idiopathic pernio, which is more likely to be reported due to detection bias, given the large amount of recent media coverage about this finding.
Neither detection bias nor a cold spring in the United States can explain the fact that cases are occurring in warm climates in individuals with positive SARS-CoV-2 viral swabs or serologies. A second unrelated infectious trigger causing a surge in pernio, while possible, seems far-fetched.
COVID-associated pernio is treated with the same drugs used for idiopathic pernio. These include high-potency corticosteroids, aspirin, topical calcium channel blockers such as nifedipine, and nitroglycerin paste. All of these uses are off-label.
Decisions in patients with COVID-related skin manifestations plus other characteristic symptoms (eg, cough, fever, shortness of breath, anosmia, loss of taste) or known COVID exposure are easy. They should be tested via nasopharyngeal swab and serologies.
In contrast, those with suspicious skin manifestations who are otherwise asymptomatic, especially with no other risk factors, fall into a gray area. Should such individuals be tested? Should they self-quarantine? To date, there is no clear consensus.
Thanks to coordinated efforts such as the nationwide consensus study in Spain and the American Academy of Dermatology's COVID-19 Dermatology Registry, we can anticipate a better understanding of how and why SARS-CoV-2 affects the skin. Hopefully, these insights will shed light on why this pathogen is so deadly for some and yet mild or asymptomatic in others.
Graeme M. Lipper, MD, is a clinical assistant professor at the University of Vermont Medical College in Burlington, Vermont, and a partner at Advanced DermCare in Danbury, Connecticut.